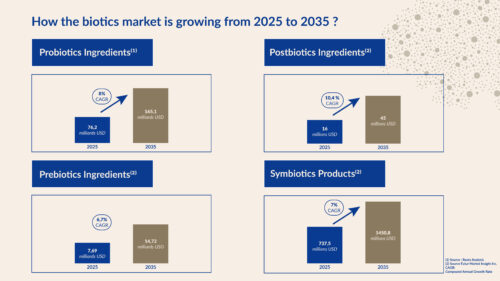
The world is becoming familiar with probiotics, prebiotics, postbiotics, and synbiotics, which could well revolutionize the field of health and wellness! According to a report by Roots Analysis[1] , the global probiotics market is expected to reach $165.1 billion by 2035, compared to $70 billion in 2024. Similarly, Future Market Insight Inc.[2] has indicated that the global prebiotics market is expected to grow from US$7.69 billion in 2023, with a compound annual growth rate (CAGR) of 6.7%, to US$14.72 billion in 2035. How can we explain such enthusiasm for these ingredients, which are found in dietary supplements, beverages, and other food products, as well as cosmetics and hygiene products?
What are prebiotics, probiotics, postbiotics, and synbiotics?
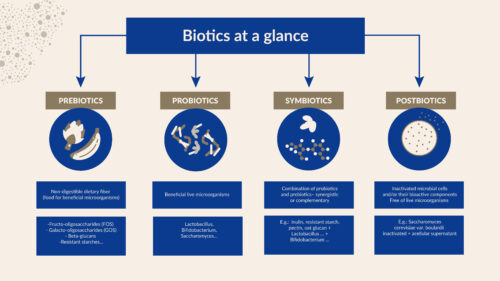
The difference between thIBSese four biotic products lies mainly in their nature and mode of action. The term “probiotic” is derived from the Greek words “pro” and “bios,” which mean “for life.” It was first discovered by Elie Metchnikoff, who found that consuming lactic acid bacteria could prolong life[3]. In 2001, the Joint Expert Advisory Panel of the Food and Agriculture Organization of the United Nations and the World Health Organization (FAO/WHO) officially defined probiotics. Later, the International Scientific Association for Probiotics and Prebiotics (ISAPP) proposed an improved definition of probiotics as “live bacteria or yeast that, when consumed in adequate amounts, have a beneficial effect on the health of the host[4]. ” Promoted by the first “active bifidus” introduced in yogurts, they are the best-known category among the general public. Whether Lactobacillus, Bifidobacteria, or conte yeast, these probiotics are widely used in cases of dysbiosis, i.e., an imbalance in the microbiota (e.g., intestinal or vaginal flora).
Prebiotics, on the other hand, refer to compounds that microorganisms feed on. In 2016, ISAPP defined prebiotics as “a substrate selectively used by host microorganisms conferring a health benefit on the host[5] .“Some are naturally present in foods, such as fiber (in fruits, vegetables, legumes, etc.) or polyphenols (in wine, red fruits, etc.). But it is also possible to consume others in the form of dietary supplements. For example, the “good” bacteria in our intestines appreciate certain yeast cell walls, which they transform through fermentation into molecules that are beneficial to health. These include butyrate, a molecule that helps modulate the immune response and limit inflammation of the intestinal wall, and propionate, a compound that may have a positive effect on metabolism. Of course, it is possible to combine a prebiotic and a probiotic, with the former enhancing the action of the latter by providing it with the nutrients it needs. This is known as a synbiotic.
In 2021, the term “postbiotics” was comprehensively described by ISAPP as “a preparation of non-living microorganisms and/or their components that confers a health benefit on the host[6] .” It includes all or part of a microorganism that has been inactivated. Effective postbiotics must contain inactivated microbial cells or cellular components, with or without metabolites, that contribute to measurable health benefits. The cell walls of yeasts used as prebiotics fall into this category, as do certain probiotic bacteria that retain their benefits once inactivated. This allows manufacturers to overcome many storage and formulation constraints that are impossible to meet for certain products or in certain regions (hot and humid countries, etc.). It can also be a safe way to work with a pathogen and use it, like an oral vaccine, to educate the intestinal immune cells.
The role of prebiotics in intestinal health
Gibson and Roberfroid first defined prebiotics in 1995 as “non-digestible food ingredients with a beneficial effect on the host by selectively stimulating the growth and/or activity of one or a limited number of bacteria in the colon”[7]. Common examples include inulin, fructo-oligosaccharides (FOS), galacto-oligosaccharides (GOS), pectin, and lactulose. Produced using a simpler process, Saccharomyces yeast walls, which consist mainly of mannoproteins and β-glucans, are also recognized as excellent prebiotics, even at low doses.
Dr. Karen Scott of the Rowett Institute in Scotland pointed out that:
“Prebiotics selectively feed beneficial bacteria, but their impact depends on diet. If there is a lack of variety, a prebiotic supplement can help maintain intestinal balance.”
Prebiotics feed the beneficial bacteria present in the gut. As human enzymes do not digest them, they pass through the digestive tract and arrive intact in the colon[8]. There, they are fermented by gut bacteria, producing specific metabolites such as short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate[9]. These SCFAs promote gut health by strengthening the intestinal barrier, modulating the immune system, and reducing inflammation. Prebiotics maintain a healthy gut microbiota by selectively promoting beneficial bacteria such as bifidobacteria and lactobacilli and suppressing harmful bacteria[10].
Numerous studies have demonstrated the existence of a dialogue between the microbiota and the brain. Beyond intestinal health, prebiotics may also act on this “microbiota-gut-brain axis.” A recent clinical study showed that adopting a prebiotic-rich diet for 8 weeks could lead to improvements in overall mood and anxiety disorders[11].
The science behind probiotics: beneficial bacteria for your gut
Our gut microbiome is home to a complex community of microorganisms living in our digestive system. It consists of more than 100 trillion microbes[12] ; most are bacteria, of which more than 1,000 species are known[13] .
Probiotics have been known for over a century and there are now many different types available. Among the groups of bacteria most commonly used as probiotics are Lactobacillus, Streptococcus, Bifidobacterium, Enterococcus, and Saccharomyces cerevisiae yeast.
The mode of action of probiotics is complex and depends on specific microbial strains. Probiotics can alter the balance of the gut microbiome and compete with pathogens for nutrients and space on the intestinal wall. They can improve intestinal barrier function and modulate the immune system. Probiotics can also produce antimicrobial metabolites that directly or indirectly influence the overall health of the host[14] .
Interestingly, some probiotics (also called psychobiotics) can act on the nervous system via the gut-brain axis. Decades of research have also shown that specific strains of probiotics offer various health benefits, such as reducing antibiotic-associated diarrhea, relieving digestive disorders, including bloating, relieving colic symptoms in babies, improving eczema, improving lactose digestion, reducing the risk or duration of upper respiratory tract infections, and more[15]. In the context of irritable bowel syndrome (IBS), which affects 5% of the world’s population, based on the number of clinical trials conducted, the number of patients treated, and the consistency of the results, the Saccharomyces Cerevisiae I-3856 (IbSium) strain is currently the leading probiotic recommended for abdominal pain[16].
What are postbiotics and why are they important?
Postbiotics, metabolic products and cellular components of probiotics, are characterized by being inert while retaining biological activity. They have the advantage of being more stable and resistant to heat, gastric acid, and digestive enzymes than certain probiotics. The exact composition of postbiotics depends on the probiotic strain, growth conditions, and substrates available for fermentation[17]. Rich in bioactive compounds such as bacteriocins, cell wall components, enzymes, exopolysaccharides, organic acids, and short-chain fatty acids, postbiotics contribute to intestinal health by strengthening the intestinal barrier, reducing inflammation, and modulating the immune system. Postbiotics can also help maintain a balanced microbiota by inhibiting harmful bacteria and promoting beneficial microbes. In addition, certain postbiotic compounds, such as SCFAs, act as signaling molecules that influence the host’s metabolism and immune responses.
Critically, the bioactivity of postbiotics depends on preparation processes, particularly inactivation methods[18] .
Dr. Gabriel Vinderola and Professor Salminen stated:
“Postbiotics are a source of many health benefits, just like probiotics. Their mode of action mainly involves activation of the immune system and interactions with host cells. The inactivation process is crucial, as changes can alter their effects, requiring clinical validation.”
Since postbiotics do not require live microorganisms, they offer advantages in terms of safety, shelf life, and ease of use in food formulations and dietary supplements. In recent years, they have attracted considerable interest due to their potential roles in immune regulation, anti-inflammation, antioxidant activity, antibacterial activity, and improvement of gut health[19].
Can prebiotics, probiotics, and postbiotics be taken together?
Yes, it is best to take probiotics and prebiotics together. This combination is often referred to as “synbiotics” and may offer more benefits. However, it should be noted that different strains of probiotics require different types of prebiotics as food. Therefore, taking a random combination of probiotics and prebiotics does not always work. Research is ongoing to find the best combinations of probiotics and prebiotics to maximize health benefits[20]. In addition to dietary supplements combining prebiotics and probiotics, consuming probiotics with foods rich in prebiotics such as bananas, onions, garlic, and oats can also promote their survival and colonization in the gut.
It should be noted that it is not necessary to take prebiotics for probiotics to work, but they can enhance their effectiveness by feeding the good bacteria. While prebiotics and probiotics have been the subject of numerous studies, their combination with postbiotics has been less explored and is not yet common.
The benefits of prebiotics, probiotics, and postbiotics for overall health
Our gut is home to billions of microbes that have a wide-ranging influence, from digestion to immunity to metabolic health. Supporting these microbes with prebiotics, probiotics, and postbiotics can offer powerful health benefits. For example, Cani et al. (2009) found that prebiotics restored intestinal barrier integrity and reduced inflammation in obese, diabetic mice in by increasing tight junction proteins and decreasing systemic inflammatory markers[21]. Interestingly, Wu et al. (2017) showed that certain prebiotics, particularly non-digestible oligosaccharides, can directly influence host immune signaling pathways, such as MAPK and NF-κB, independently of the microbiota. This dual action, both microbial and host-directed, enhances their health potential[22]. Using a state-of-the-art dynamic model for simulating the gut microbiota (PolyFermS®) ,Lesaffre Science & Technology (LIST) has also demonstrated that a patented ingredient based on yeast cell walls, Lynside ® Immunity Prebiotic, has a prebiotic effect and stimulates, even at low doses (500 mg to 1 g/day), the dominant bacterial family of the intestinal flora. “Its innovation lies in its personalized action. The composition of the gut microbiota can vary from one individual to another. While other prebiotics on the market target a specific group of bacteria (such as lactobacilli), this one adapts to each microbiota, consolidating the base of its bacterial population to strengthen its ability to protect the body,” explains Clarisse Geraci, Prebiotics Product Manager at Gnosis by Lesaffre. The unique feature of this prebiotic is that it adapts to the diversity of the microbiota, induces the production of specific SCFAs, and is thus able to support immune function.
Probiotics do not only act in the intestine: they also contribute to the proper functioning of the immune system by strengthening the activity of defense cells and limiting inflammatory reactions. The Bacillus subtilis CNCM I-2745 strain, for example, strengthens the immune system by increasing sIgA antibody levels in the intestine and saliva, playing a key role in protecting against pathogens. A clinical study has shown that it reduces the frequency of respiratory infections in seniors by up to 45%[23].
Thanks to the gut-brain connection, they can also have a positive impact on emotional balance and help to better manage stress. For skin health, topical probiotics have shown beneficial effects in the treatment of certain inflammatory skin conditions such as acne, rosacea, psoriasis, etc., and their role in wound healing has also shown promise [24].
In terms of metabolism, probiotics influence blood sugar regulation and could therefore play a role in weight control. They also have an effect on cardiovascular health, helping to reduce “bad” cholesterol[25,26,27,28] (LDL) and helping to stabilize blood pressure. In addition, probiotics play a role in balancing the oral microbiota, thereby reducing the risk of infections and improving oral health[29].
For vaginal health, the patented probiotic yeast CNM I-3856 has clinically proven efficacy in cases of bacterial and fungal vaginosis. The Lesaffre Institute of Science & Technology (LIST) has also shown that the combination of certain strains of Lactobacillus and S.cerevisiae CNCM I-3856 co-aggregates with the pathogen C.Albicans, preventing it from attaching to and colonizing mucous membranes[30]. Given the emergence of antifungal resistance, this solution could become a potential therapeutic alternative.
A recent study has also shown that the administration of the bacterium Akkermansia muciniphila, a new-generation probiotic due to its metabolic and immunomodulatory effects, is able to counteract the deleterious effects of food emulsifiers such as carboxymethylcellulose and polysorbate 80[31]. Indeed, certain emulsifiers used by the food industry to improve texture and extend the shelf life of processed products can lead to alterations in the gut microbiota.
Considered as potential alternatives to probiotics, postbiotics are attributed with various bioactivities detailed in a recent literature review[33] . Among the many benefits cited depending on their bioactive composition, the following are particularly noteworthy:
- At the intestinal level, antioxidant, anti-inflammatory, antidiabetic, immunomodulatory, antihypertensive, and antimicrobial properties,
- Systemic effects, i.e., effects that influence the entire body, such as preventing or reducing obesity, slowing abnormal cell growth (linked to cancer prevention), lowering blood pressure, and reducing cholesterol.
Developing in a relatively undefined regulatory landscape, postbiotics are already being marketed as dietary supplements with a wide range of indications, including:
- supporting the immune system in the intestinal tract,
- supporting metabolic balance in overweight individuals,
- supporting metabolic balance in people with chronic fatigue,
- reducing the bacterial load of Helicobacter pylori (a risk factor for ulcers and gastritis),
- promoting digestive health by improving the structure of intestinal villi and protecting against inflammation, oxidative stress, and disruption of the intestinal barrier.
- stimulates the restoration of intestinal flora
- helps reduce stress, improve mood, and optimize sleep efficiency,
- combats visual fatigue.
Despite encouraging results regarding the health benefits of postbiotics, future research will clarify the specific roles of different postbiotic components.
See also: Postbiotics: a missing key to supporting gut health?
How to incorporate prebiotics, probiotics, and postbiotics into your diet
Experts recommend consuming fermented foods (containing probiotics) to promote diversity in the gut microbiome and foods rich in fiber (i.e., prebiotics) to nourish and maintain beneficial bacteria. Foods rich in probiotics commonly cited include yogurt, kefir, kombucha, cheese, uncooked sauerkraut, kimchi, and pickles. Note that beer, wine, sourdough bread, chocolate, and coffee, although fermented foods, do not contain live microorganisms.
Prebiotics are naturally present in fiber-rich vegetables, fruits, and whole grains such as onions, garlic, asparagus, leeks, Jerusalem artichokes, apples, green bananas, oats, and barley[33] . It should be noted that beverages enriched with prebiotics, particularly in the soda category, are becoming increasingly popular. In 2025, Pepsico launched Pepsi® Prebiotic Cola, which provides 3 g of prebiotic fiber per 35cl can.
Fermented foods are rich in inactivated microbial cells, components, and metabolites, which contribute to postbiotic benefits. You can naturally stimulate the presence of postbiotics in your body by increasing your consumption of foods rich in probiotics and prebiotics.
Probiotics and prebiotics are now widely consumed in the form of dietary supplements, which come in various forms (capsules, tablets, granules, powders, liquids) or medical devices (vaginal ovules, suppositories, nasal sprays). Probiotic supplements often contain between 1 and 10 billion CFU per dose, with some reaching 50 billion CFU or more. A 2017 review of the dose-response relationship in several meta-analyses concluded that a dose of 10 billion CFU/day was an adequate threshold for preventing antibiotic-associated diarrhea[34] .
According to ISAPP, most intestinal prebiotics such as inulin, fructooligosaccharides (FOS), galactooligosaccharides (GOS), and human milk oligosaccharides (HMO) require an oral dose of at least 3 grams per day or more to be effective.[35] . However, in the case of prebiotic yeasts such as Lynside Immunity, 500 mg is sufficient to be effective, i.e., 2 capsules per month for 2 months.
See also: Cocoa fermentation: the key to delicious chocolate
See also: What is the best coffee?
Common myths about prebiotics, probiotics, and postbiotics debunked
Several common myths about prebiotics, probiotics, and postbiotics need to be debunked.
Myth: All probiotics offer the same health benefits, regardless of the strain or formulation.
Reality: This is simply not true. In fact, each probiotic strain has unique properties and functions. The properties of a probiotic are carried by a given strain, not by the species and even less by the genus. For example, the strain S. boulardii CNCM I-3799 is recommended for the treatment and prevention of diarrhea[36] ,while S. cerevisiae CNCM I-3856 helps improve intestinal comfort (bloating, transit disorders, etc.[37].
Probiotic microorganisms must also be present in sufficient quantities: at least 109to 1011CFU per daily dose. However, it is important to note that neither the presence of multiple strains nor the number of bacteria/yeasts is sufficient to prove a product’s effectiveness. It is therefore advisable to check whether there is sufficient scientific evidence (clinical studies by example) confirming the preventive or therapeutic effects of each of the strains considered at the recommended dose.
Given that probiotics are living organisms, their viability and therefore their effectiveness can be affected by various environmental stresses, such as gastric acidity, bile salts and other digestive enzymes, cervical mucus, humidity, temperature, and oxidation. This is why the dosage form and formulation must guarantee:
- clearly identified strains of bacteria or yeast with scientifically proven effects,
- the survival of probiotics in the digestive tract (gastro-resistance) or the vaginal or nasal environment, depending on the mode of administration,
- a recommended dose, which must be based on the induction of the claimed physiological effect,
- a number of live probiotic strains until the end of the product’s shelf life.
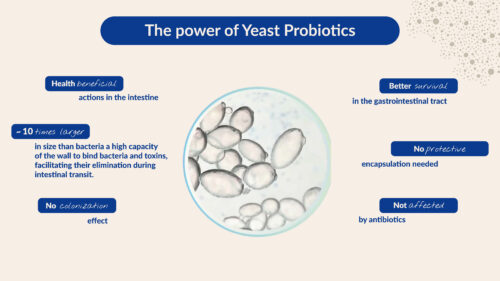
It should be noted that studies have reported higher tolerances of probiotic yeasts to body temperature (37°C) and acid stress (pH 3), which ensure better viability in the gastric environment [38] .
Myth: Probiotics are only beneficial for intestinal health.
Reality: Although gut health is a priority, probiotics can influence various aspects of health, including immunity, skin, mental health, and metabolism. Prescribing probiotics may be useful in the following cases:
- Functional bowel disorders, such as abdominal pain, flatulence (…) in the context of irritable bowel syndrome (IBS)
- Treatment and prevention of diarrhea
- Inflammatory bowel disease (IBD)
- Maintaining intestinal microflora after taking antibiotics
- Helicobacter pylori infection
- Prevention of allergies and eczema
- Lactose intolerance
- Vaginal infections
- Upper respiratory tract infections (such as colds) or intestinal infections
- Support for oral health (periodontal disease and bad breath)
Myth: Fermented foods are the same as probiotics.
Truth: Although fermented foods such as yogurt, raw sauerkraut, kombucha, or kefir contain live microbes, they do not necessarily meet the scientific criteria to be classified as probiotics. They are certainly a source of beneficial microorganisms, but until controlled studies have demonstrated that certain strains have positive effects on health, they cannot be considered true probiotics.
Myth: Probiotics can solve all digestive problems.
Reality: Probiotics can be beneficial in certain specific situations, but they do not solve all digestive problems. Their use must be tailored to the individual case and ideally discussed with a healthcare professional. Their effectiveness depends on the specific strain, the dose, and the clinical context.
Myth: Prebiotics are only useful for digestion.
Reality: Prebiotics are non-digestible fibers that serve as food for good intestinal bacteria. They promote digestive function and regulate intestinal transit, but their benefits go beyond intestinal health. By promoting a healthy microbiota, prebiotics can also support:
- Immune health,
- mineral absorption (such as calcium),
- Metabolic health, such as better blood sugar control,
- Mental health (stress, anxiety, depression).
Myth: Postbiotics are just dead probiotics, so they don’t do anything.
Reality: Postbiotics do not reproduce, but they are not inactive. They contain bioactive compounds such as short-chain fatty acids, proteins, vitamins, enzymes , peptides, and inactivated microbial cells that can stimulate the immune system, reduce inflammation, strengthen the intestinal barrier, and influence metabolic functions.
Myth: If a probiotic product expires, it automatically becomes a postbiotic.
Reality: A postbiotic is intentionally produced through the controlled inactivation of microbes and validated by clinical studies. Expired probiotics may no longer contain beneficial compounds and have not been tested for safety or efficacy in their degraded form.
Side effects and potential risks of prebiotics, probiotics, and postbiotics
Prebiotics, probiotics, and postbiotics can cause side effects, especially if used incorrectly. Their safety is important to consider, particularly for immunocompromised individuals, critically ill patients, children, and people with central venous catheters. Probiotics can cause four side effects in vulnerable individuals: infections, harmful metabolic activities, excessive stimulation of the immune system, and gene transfer, although infections are rare [39]. Bacteria-based probiotics can cause temporary gas and bloating[40] ,while yeast-based probiotics can cause constipation and increased thirst[41]. Abdominal pain and diarrhea usually occur at high doses[42] ,but should disappear within a few weeks. Certain probiotic strains, such as Lactobacillus buchneri, Lactobacillus helveticus, Lactobacillus hilgardii, and Streptococcus thermophilus, can produce high levels of histamine, which may cause allergic reactions in people who are histamine intolerant[43,44,45]. Prebiotics may also cause digestive upset, bloating, or diarrhea, especially in sensitive individuals[46]. One study suggests that high prebiotic intake may intensify IBS symptoms due to the high carbohydrate content of many prebiotic-rich foods[47].
The Future of Biotics
Recent discoveries about the microbiome and advances in sequencing and culture methods are transforming the future of probiotics and prebiotics[48] . Long limited to lactobacilli and bifidobacteria, probiotics now include promising new species from the human microbiome, such as Oseburia intestinalis, Eubacterium spp., Akkermansia muciniphila, and Faecalibacterium prausnitzii. Known as new generation probiotics (NGPs), they could have therapeutic or prophylactic applications. However, their use poses technical challenges, particularly the production and preservation of sensitive anaerobic bacteria. Thanks to the ongoing development of synthetic biology, it is now possible to design probiotics with the characteristics and functionalities desired for human health. Genetically modified probiotic strains could, for example, deliver therapeutic agents and target specific sites in the intestine.
At the same time, prebiotics traditionally derived from plant fibers are expanding to new sources such as polyphenols and oligosaccharides from breast milk. The combination of prebiotics and probiotics gives rise to synbiotics, sometimes designed in consortia to maximize effects.
Finally, postbiotics, derived from inactivated microorganisms, are emerging as a more stable and safer alternative. For example, the bacterium Akkermansia muciniphila, whether live or pasteurized, improves several metabolic parameters, particularly in cases of obesity and type 2 diabetes, and is recognized as a novel food by the EFSA as a postbiotic[49] .
These innovations could transform the prevention and treatment of intestinal diseases, and even beyond, with health prospects ranging from metabolic and liver diseases to mood disorders, obesity, and hypercholesterolemia. Thanks to the advent of personalized nutrition and precision medicine, as well as research consortiums supported by Lesaffre, such as Ferment du Futur and French Gut, will it be possible in the future to model and predict changes in the gut microbiota associated with different diseases or disorders, and to offer new food products and personalized solutions based on biotics?
Frequently Asked Questions (FAQ)
- What is the difference between prebiotics, probiotics, and postbiotics?
Whether prebiotics, probiotics, or postbiotics, they must confer a health benefit on the host when consumed in sufficient quantities. Prebiotics are non-digestible food components, mainly fibers, which serve as food for the microorganisms present in our microbiota (intestines, vagina, skin). Probiotics are beneficial live bacteria or yeasts known for their health benefits. Postbiotics consist of dead microorganisms (intact or fragmented) with or without their metabolites.
- How long does it take for probiotics to work?
The time it takes for probiotics to produce visible effects varies depending on several factors, including the specific strain used, the person’s health status, and the reason for supplementation. Some people may see improvements within a few days, while others may take several weeks. It is essential to maintain regular use and consult a healthcare professional for personalized advice.
- Can I take prebiotics and probiotics together?
Yes, taking prebiotics and probiotics together is safe and can be particularly beneficial. This combination is often referred to as “synbiotics.” Prebiotics serve as food for probiotics, promoting their growth and activity, which can improve gut health and overall well-being. The World Gastroenterology Organization (WGO) states that the optimal dose of probiotics depends on the strain and product and recommends that clinicians advise their patients to use only strains, doses, and treatment durations that have been shown to be beneficial in human studies.
- What are the best foods for stimulating my gut microbiota?
Eating a healthy and varied diet in balanced quantities will have a positive influence on your gut microbiota. So don’t hesitate to eat these three categories of foods that are particularly beneficial for your microbiota.
- Fiber-rich foods: whole grains, fruits, and vegetables are rich in dietary fiber, which acts as a prebiotic, promoting the growth of beneficial bacteria.
- Fermented foods: Foods such as yogurt, raw sauerkraut, kimchi, and kefir contain live probiotics that can improve the diversity of the gut flora.
- Foods rich in polyphenols: Polyphenols in antioxidant-rich fruits, vegetables, and oilseeds modulate the gut microbiota, a role that complements their main antioxidant and anti-inflammatory properties [50] .
Conclusion
As we have seen, probiotics, prebiotics, postbiotics, and synbiotics are among the most promising concepts for human health. But did you know that these biotics are also gaining momentum in animal health and welfare? Drawing on its research ecosystem and strategic partnerships, Lesaffre and its business units Gnosis by Lesaffre and Phileo by Lesaffre are highlighting the potential of microorganisms and developing innovative approaches to human and animal health.
References:
- https://www.rootsanalysis.com/reports/probiotics-market.html
- https://www.futuremarketinsights.com/reports/prebiotic-ingredient-market
- Podolsky, S. H. (2012). Metchnikoff and the microbiome. Lancet North Am Ed, 380(9856), 1810–1811.
- Hill, C., et al. (2014). The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nature Reviews Gastroenterology & Hepatology, 11(8), 506–514.
- Gibson, G. R., et al. (2017). Expert consensus document: The ISAPP consensus statement on the definition and scope of prebiotics. Nature Reviews Gastroenterology & Hepatology, 14(8), 491–502.
- Salminen, S., et al. (2021). The ISAPP consensus statement on the definition and scope of postbiotics. Nature Reviews Gastroenterology & Hepatology, 18(9), 649–667.
- Gibson, G. R., & Roberfroid, M. B. (1995). Dietary modulation of the human colonic microbiota: Introducing the concept of prebiotics. Journal of Nutrition, 125(6), 1401–1410.
- Bindels, L. B., Delzenne, N. M., Cani, P. D., & Walter, J. (2015). Towards a more comprehensive concept for prebiotics. Nature Reviews Gastroenterology & Hepatology, 12(5), 303–310.
- Koh, A., De Vadder, F., Kovatcheva-Datchary, P., & Bäckhed, F. (2016). From dietary fiber to host physiology: Short-chain fatty acids as key bacterial metabolites. Cell, 165(6), 1332–1345.
- Barratt, M. J., Nuzhat, S., Ahsan, K., et al. (2022). Bifidobacterium infantis treatment promotes weight gain in Bangladeshi infants with severe acute malnutrition. Science Translational Medicine, 14(640), eabk1107.
- Freijy Tania M. et al, (2023), Effects of a high-prebiotic diet versus probiotic supplements versus synbiotics on adult mental health: The “Gut Feelings” randomised controlled trial, Front. Neurosci., 06 February 2023, Volume 16 – 2022 | https://doi.org/10.3389/fnins.2022.1097278
- Koh, A., De Vadder, F., Kovatcheva-Datchary, P., & Bäckhed, F. (2016). From dietary fiber to host physiology: Short-chain fatty acids as key bacterial metabolites. Cell, 165(6), 1332–1345.
- Barratt, M. J., Nuzhat, S., Ahsan, K., et al. (2022). Bifidobacterium infantis treatment promotes weight gain in Bangladeshi infants with severe acute malnutrition. Science Translational Medicine, 14(640), eabk1107.
- Sanders, M. E., et al. (2013). An update on the use and investigation of probiotics in health and disease. Gut, 62(5), 787.
- Ji, J., et al. (2023). Probiotics, prebiotics, and postbiotics in health and disease. MedComm, 4(6), e420.
- Vivek C. Goodoory, Mais Khasawneh, Christopher J. Black, Eamonn M.M. Quigley, Paul Moayyedi, Alexander C. Ford, Efficacy of Probiotics in Irritable Bowel Syndrome: Systematic Review and Meta-analysis, Gastroenterology, Volume 165, Issue 5, 2023, Pages 1206-1218, ISSN 0016-5085,? https://doi.org/10.1053/j.gastro.2023.07.018
- Vinderola, G., Sanders, M. E., & Salminen, S. (2022). The concept of postbiotics. Foods, 11(8), 1077.
- Zhu, Y.; Xiao, M.; Kang, T.; He, Y.; Zhang, J.; Zhao, Y.; Xiao, X. The role of inactivation methods in postbiotic composition and bioactivity modulation: a review. Foods 2025, 14, 2358. https://doi.org/10.3390/foods14132358
- Rafique, N., et al. (2023). Promising bioactivities of postbiotics: A comprehensive review. Journal of Agriculture and Food Research, 14, 100708.
- Gomez Quintero, D. F., Kok, C. R., & Hutkins, R. (2022). The future of synbiotics: Rational formulation and design. Frontiers in Microbiology, 13, 919725.
- Cani, P. D., et al. (2009). Changes in gut microbiota control inflammation in obese mice through a GLP-2-driven mechanism. Gut, 58, 1091–1103.
- Wu, R. Y., et al. (2017). Non-digestible oligosaccharides regulate host kinome to modulate inflammatory responses. Microbiome, 5, 135
- Lefevre M, Racedo SM, Ripert G, Housez B, Cazaubiel M, Maudet C, Jüsten P, Marteau P, Urdaci MC. Probiotic strain Bacillus subtilis CU1 stimulates immune system of elderly during common infectious disease period: a randomized, double-blind placebo-controlled study. Immun Ageing. 2015 Dec 3;12:24. doi: 10.1186/s12979-015-0051-y.
- Habeebuddin M, Karnati RK, Shiroorkar PN, Nagaraja S, Asdaq SMB, Khalid Anwer M, Fattepur S. Topical Probiotics: More Than a Skin Deep. 2022 Mar 3;14(3):557. doi: 10.3390/pharmaceutics14030557.
- Cavallini, D. C. U., et al. (2016). Probiotic soy product with isoflavones improves lipid profile: A randomized trial. Nutrients, 8, 52.
- Park, S., et al. (2018). Lactobacillus rhamnosus BFE5264 lowers cholesterol and alters gut microbiome. PLoS ONE, 13, e0203150.
- Peters, V. B. M., et al. (2019). Mechanisms and immunomodulatory properties of pre- and probiotics. Beneficial Microbes, 10, 225–236.
- Jones, M. L., et al. (2012). Cholesterol-lowering efficacy of Lactobacillus reuteri yoghurt formulation. British Journal of Nutrition, 107, 1505–1513.
- Inchingolo, F.; Inchingolo, A.M.; Malcangi, G.; De Leonardis, N.; Sardano, R.; Pezzolla, C.; de Ruvo, E.; Di Venere, D.; Palermo, A.; Inchingolo, A.D.; et al. The Benefits of Probiotics on Oral Health: Systematic Review of the Literature. Pharmaceuticals 2023, 16, https://doi.org/10.3390/ph16091313
- Spacova, I., Allonsius, C.N., De Boeck, I. et al. Multifactorial inhibition of Candida albicans by combinations of lactobacilli and probiotic Saccharomyces cerevisiae CNCM I-3856. Sci Rep 14, 9365 (2024). https://doi.org/10.1038/s41598-024-59869-9
- Daniel N, Gewirtz AT, Chassaing B? Akkermansia muciniphila counteracts the deleterious effects of dietary emulsifiers on microbiota and host metabolism? Gut 2023;72:906-917.
- Amobonye, A., Pillay, B., Hlope, F. et al. Postbiotics: an insightful review of the latest category in functional biotics. World J Microbiol Biotechnol 41, 293 (2025). https://doi.org/10.1007/s11274-025-04483-8
- Davani-Davari, D., et al. (2019). Prebiotics: Definition, types, sources, mechanisms, and clinical applications. Foods, 8(3), 92.
- Ouwehand, A. C. (2017). A review of dose-responses of probiotics in human studies. Beneficial Microbes, 8(2), 143–151.
- https://isappscience.org/for-scientists/resources/prebiotics/
- https://www.efsa.europa.eu/en/efsajournal/pub/2801
- Spiller, R., Pélerin, F., Cayzeele Decherf, A., Maudet, C., Housez, B., Cazaubiel, M., & Jüsten, P. (2016). Randomized double-blind placebo-controlled trial of Saccharomyces cerevisiae CNCM I-3856 in irritable bowel syndrome: improvement in abdominal pain and bloating in those with predominant constipation. UEG Journal, 4: 353-362. https://doi.org/10.1177/2050640615602571
- https://www.tandfonline.com/doi/full/10.2147/IJN.S337427#abstract
- Kothari, D., Patel, S., & Kim, S. K. (2019). Probiotic supplements might not be universally effective and safe. Biomedicine & Pharmacotherapy, 111, 537–547.
- Williams, N. T. (2010). Probiotics. American Journal of Health-System Pharmacy, 67(6), 449–458.
- Karpa, K. D. (2007). Probiotics for Clostridium difficile diarrhea: A perspective. Annals of Pharmacotherapy, 41(7–8), 1284–1287.
- Merenstein, D., et al. (2023). Emerging issues in probiotic safety: 2023 perspectives. Gut Microbes, 15(1), 2185034.
- Gezginc, Y., et al. (2013). Biogenic amines in Streptococcus thermophilus from yogurt. Food Chemistry, 138(1), 655–662.
- Rossi, F., et al. (2011). Histamine production by S. thermophilus PRI60 in cheese conditions. Applied and Environmental Microbiology, 77(8), 2817–2822.
- Joosten, H. M. L. J., & Northolt, M. D. (1989). Amine-producing lactobacilli in cheese. Applied and Environmental Microbiology, 55(9), 2356–2359.
- Marteau, P., & Seksik, P. (2004). Tolerance of probiotics and prebiotics. Journal of Clinical Gastroenterology, 38(Suppl), S67–S69.
- Whelan, K. (2013). Mechanisms and effectiveness of prebiotics in digestive disorder management. Proceedings of the Nutrition Society, 72(3), 288–298.
- Marla Cunningham, M. Andrea Azcarate-Peril, Alan Barnard, Valerie Benoit, Roberta Grimaldi, Denis Guyonnet, Hannah D. Holscher, Kirsty Hunter, Sarmauli Manurung, David Obis, Mariya I. Petrova, Robert E. Steinert, Kelly S. Swanson, Douwe van Sinderen, Jelena Vulevic, Glenn R. Gibson, Shaping the Future of Probiotics and Prebiotics, Trends in Microbiology, Volume 29, Issue 8, 2021, Pages 667-685, https://doi.org/10.1016/j.tim.2021.01.003.
- https://www.efsa.europa.eu/en/efsajournal/pub/6780
Plamada D, Vodnar DC. Polyphenols-Gut Microbiota Interrelationship: A Transition to a New Generation of Prebiotics. Nutrients. 2021 Dec 28;14(1):137. doi: 10.3390/nu14010137. PMID: 35011012; PMCID: PMC8747136.


